Pelvic floor dysfunction (PFD) isn’t pleasant! But if you’re suffering from it (or suspect you are), then you’ve come to the right place to get information about it and get it treated.
So what are the symptoms?
It can cause awkward sensations, such as difficulty urinating or frequently needing to use the bathroom. Worse still, you may experience decreased sexual sensation or painful intercourse, leading to your sex life suffering big time.
It can be difficult to talk about, but if there’s any area in your life where you should put your cards on the table, it’s the issues surrounding pelvic floor dysfunction.
It’s wise to address PFD in its mild form before it starts causing you more difficulties, especially when you consider that the PFD symptoms can progressively worsen.
Luckily, here at nixit, we welcome all topics under the sun, and the good news is, if you catch PFD early on, there's many effective treatments that can get your life back on track.
Today we talk about what pelvic floor dysfunction is, what the most common symptoms and causes are, and the treatment options.
What Is Pelvic Floor Dysfunction?
Pelvic floor dysfunction can be an umbrella of different disorders - from pelvic organ prolapse to difficulty passing stool and urine. These disorders indicate your pelvic floor may not be doing its job effectively.
To understand this further, let’s go back to the basics. The pelvic floor is the entire area surrounding your pelvic bone: muscles, ligaments, and tissues included. The muscles reach from the front of your pelvic bone to the lowest part of your spine (called the sacrum), attaching to all sides of the pelvic bone.
The muscles must be able to contract and relax to work properly and carry out their primary function of keeping your vagina, bladder, and rectum in place. So pelvic floor disorders crop up when pelvic floor muscles start to fall behind in performing these functions. Let’s examine which symptoms these disrupted functions can bring about.
What Are the Symptoms?
People suffering from PFD can have weak or overly strong pelvic floor muscles. So, you can expect different symptoms depending on which of these two conditions you have. In medical jargon, pelvic floor disorders are divided into low and high-tone disorders. In other words, you can have a hypertonic pelvic floor or a hypotonic pelvic floor.
If your pelvic muscles are low-tone, they get more relaxed and looser than usual. As a result, you may have difficulty contracting them. When this happens, your core cannot be adequately supported, leading to urinary and bowel incontinence and pelvic organ prolapse.
On the flip side, if your pelvic floor muscles have a high-tone, they’re tighter and more restricted than usual, and you're likely to have trouble relaxing them. As a result, you may experience pain upon trying to relax or stretch these muscles.
High-tone pelvic muscles can also create problems with urinating and emptying your bowel and bladder, as well as a whole load of other related issues such as muscle spasms, pelvic pain, and painful intercourse.
With that in mind, let’s take a look at some of the symptoms.
Causes of Pelvic Floor Dysfunction
Looking at the possible causes of pelvic floor dysfunction makes sense for two reasons: you know what issues are causing your ailment and you know whether you have a greater risk of developing PFD than other people.
Like we did before, we’ll parse the information on PFD causes into those affecting high and low pelvic floor disorders.
Common Causes Of Low-tone Pelvic Floor Disorders:
- Pregnancy.
- Chronic constipation (bearing down too hard while emptying your bowel can weaken your pelvic floor muscles).
- Sustained traumatic injuries to the pelvic region.
- Advancing age.
- Drops in estrogen levels during menopause.
- Pelvic surgery.
Pro Tip: The most common cause of PFD is childbirth and pregnancy. Pelvic muscles tend to weaken immediately after labor. And though the loss of control and sensation in your pelvic region (often followed by trouble controlling your bladder and bowel movements) is distressing, these issues can be amended by physical therapy.
Common Causes Of High-Tone Pelvic Floor Disorders:
- Scar tissue.
- Endometriosis (chronic pain and inflammation in the pelvis can get your muscles to tighten protectively).
- Birth trauma (the pain and scarring caused by vaginal tearing can create tension in the pelvic floor area).
- History of holding urine or stool.
- Irritable bowel syndrome.
- Fibromyalgia.
- Hemorrhoids.
What Are the Treatment Options for Pelvic Floor Disorders?
(Image source: Pexels)
We’d all rather skip having to deal with a pelvic prolapse or urinary incontinence, but roughly one-third of AFAB will experience prolapse at some point during their lifetime.
Yet it’s not all doom and gloom either. Mild cases may not require any treatment, while more severe ones may require treatment and even surgery.
That said, it’s paramount to talk to your healthcare provider, so you devise an appropriate treatment option.
The good news is there are many therapeutic approaches for treating pelvic floor dysfunction, including:
- Pelvic floor rehabilitation. Your therapist will perform a manual examination to diagnose your condition and isolate a group of problematic muscles. They may perform pelvic floor massage, equip you with a list of physical exercises to help condition your pelvic muscles, or prescribe electrical neural stimulation.
- Biofeedback. A therapist will insert special sensors into your pelvic floor area to teach you how to retrain them.
- Dietary changes. Making dietary changes can go a long way in helping with bowel movements. These typically include drinking more fluids and adding more fiber to your diet.
- Kegel exercises. Kegels are physical exercises that focus on conditioning a specific group of muscles in your pelvic floor. Pelvic floor muscle improves muscle contraction and includes contracting and relaxing the pelvic floor muscles interchangeably.
- Vaginal dilators. These specialized plastic tube-shaped instruments are used to treat the hypotonicity of the pelvic floor. They’re used to stretch and relax vaginal muscles and involve using different size dilators gradually at the patient’s own pace.
- Pessary. A pessary can be used in more advanced cases of hypertonicity of the pelvic floor. It’s a device inserted into your vagina to help support prolapsed organs.
- Surgery. Surgery is a last resort in treating PFD, but a doctor may recommend it if this condition starts interfering with your daily life.
FAQs
Can Pelvic Floor Treatments Improve Physical Sensation?
You bet! Pelvic floor treatment and physiotherapy can help boost sexual sensation in some people with a vagina, and there’s data to back up this claim.
In a 2014 study, people with the most significant increase in PFM strength and endurance experienced the greatest improvement in response to sexual stimulation.
Can Pelvic Floor Exercises Cure Incontinence?
Pelvic floor exercises, which include strengthening the pelvic floor muscles, can help relieve the symptoms of PFD, including urinary incontinence. A timely physiotherapist visit, after childbirth, for example, can help prevent future incontinence issues.
Can You Use a Menstrual Cup With Pelvic Floor Dysfunction?
Yes, you can use a menstrual cup with pelvic floor dysfunction. There’s been some conflicting talk about whether they can cause pelvic prolapse, but these arguments are based on no scientific grounds.
So, no, menstrual cups do not pose any risk of making your prolapse symptoms worse (have a look at an expert's take on this contentious issue here).
Did you know? Lauren Ohayon recommends nixit to her clients. Pretty cool!
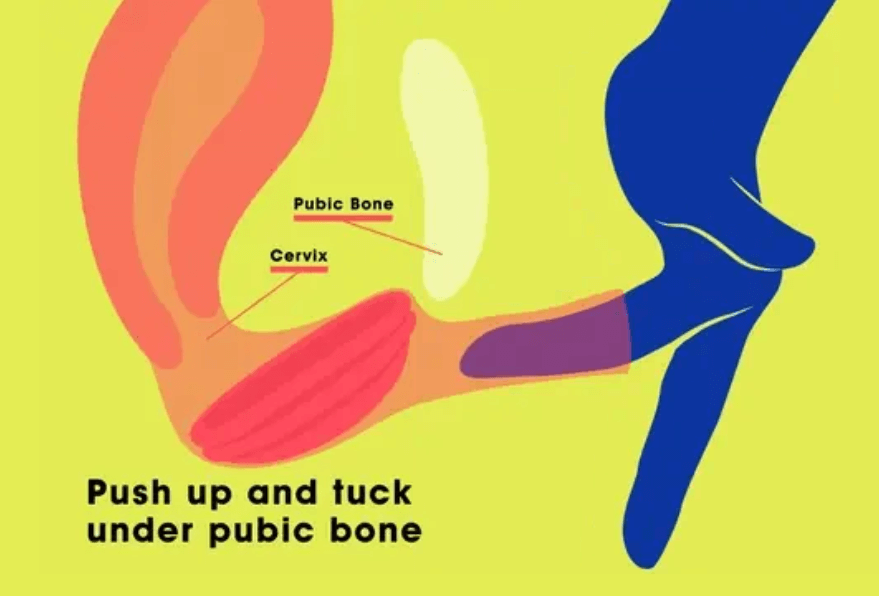
nixit offers disc-shaped menstrual cups designed with convenience and vaginal health in mind.
They’re eco-friendly, BPA-free, and suction-free. We understand some users may be unsettled about suction, so with a disc-shaped cup, there’s no pulling on your pelvic organs whatsoever.
Give Pelvic Floor Physical Therapy a Try
So, there you go. The symptoms, treatment, and factors contributing to pelvic floor dysfunction are laid out in front of you. This knowledge can be spectacularly valuable if you don’t want to allow PFD to control you.
That said, if you start suspecting something, head straight to your GP or a physiotherapist. They’ll help you treat any minor issues you may have, preventing them from worsening.
Here at nixit, our mission is to take care of your vaginal health and the environment. We also believe the taboo around reproductive health issues is causing them to be unjustifiably neglected. Be sure to explore our range of period products made by women, for women!
With that in mind, we stand behind self-literacy, seeking to normalize discussing the ins and outs of vaginal wellness. So, take a look at our archive if you want to keep learning more:
- Do Menstrual Cups Cause Pelvic Organ Prolapse? An Expert Weighs In
- What Is Pelvic Floor Therapy and What Are the Benefits
- Menstrual Disc: Your A to Z Beginner Guide
You can also visit our menstrual disc product to learn more about menstrual discs.